On September 23, Prime Minister Narendra Modi launched his government’s flagship health care program, the Ayushman Bharat-National Health Protection Mission (AB-NHPM), also called the Pradhan Mantri Jan Arogya Yojana (PMJAY), in Ranchi, the capital of the eastern state of Jharkhand. It was rolled out simultaneously in more than 450 districts across the country. Modi called it a “game changer.”
Dubbed “Modicare” by the media, the NHPM is estimated to be the biggest government-funded health insurance program globally. More than 100 million of India’s poorest families – that’s some 500 million people and about 40% of the population — will get free health coverage of Rs. 500,000 ($6,893) a year for secondary and tertiary hospitalization. The insurance will cover more than 1,350 procedures including cancer treatments, coronary bypass, angioplasty and knee replacements. It will also include charges for pre-and post-hospitalization, diagnostics, medicines, etc.
The NHPM is part of Ayushman Bharat (Healthy India), a two-pronged initiative of the Modi government. The other component focuses on setting up 150,000 health and wellness centers across the country. These will provide comprehensive primary health care including free essential drugs and diagnostic services. Modi launched the first center in April 2018. The government has allocated Rs. 1,200 crore ($165 million) to establish the centers.
The government expects the NHPM to cost around Rs. 10,000 crore to Rs. 12,000 crore ($1.3 billion to $1.6 billion) a year as of now. This will be paid for by the central and the state governments (and union territories) in 60:40 ratio. So far, 31 of the 36 state governments and union territories have signed up for it. They can choose to implement the scheme through an insurance company or directly through a trust/society or use an integrated model. The beneficiaries, who will be identified on the basis of deprivation and occupational criteria using the 2011 socio-economic caste census, will be able to access the services anywhere in the country in government hospitals and in participating private hospitals (provided that their states have signed up). What’s more, it will be a paperless and cashless transaction for them.
Modi has described the program as an “opportunity” for him “to serve the poor.” But one question looming large is whether this is simply an opportunistic move on his part. Is it a populist move driven by political considerations? India is heading for the polls next year, and a scheme like this could earn Modi both good will and votes, which in turn could translate to a second term in office. Opposition parties have been quick to slam the NHPM. The chief minister of Delhi and the national convener of the Aam Aadmi Party, Arvind Kejriwal, has dismissed it as a “PR exercise.” Congress leader P. Chidambaram has called it a “jumla” (empty promise). Santanu Sen of the Trinamool Congress party has described it as “playing to the gallery [to attract] poor people.”
“This is an incredibly ambitious scheme. There are lots of moving parts, and it’s daunting to say the least.” –Lawton R. Burns
Others say the question is not whether or not this is a populist move. Lawton R. Burns, professor of health care management at Wharton, for instance, points out: “Government health care schemes are usually designed to appeal to your base as well as to try to do the right thing. There’s nothing wrong with that.” Adds Atul Gupta, Wharton professor of health care management: “That is a common feature of democracies and not limited to this [Modi] government or even to India.”
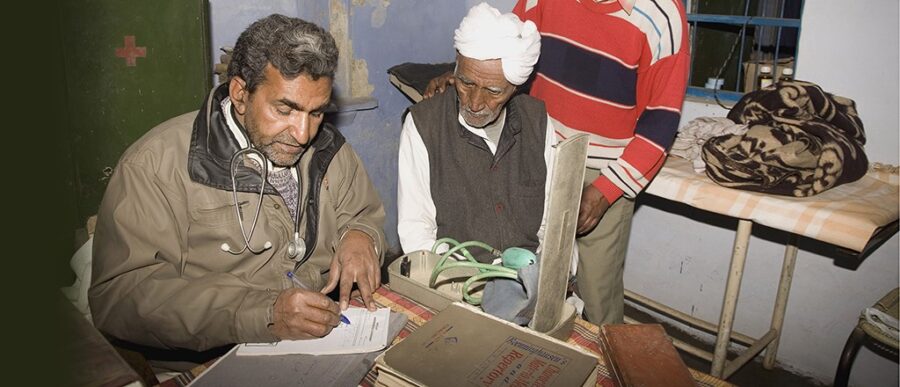
A Compelling Need
There is also no doubt that this is a much needed move for India. A report by the Confederation of Indian Industry (CII) and PricewaterhouseCoopers (PwC) on the NHPM notes that more than 80% of India’s population does not have any significant health insurance coverage. Some two-thirds of health care spending is out-of- pocket, and every year more than 60 million Indians are pushed into poverty because of medical expenses. A strong health care program is imperative to power a country’s economic development, but India has so far under-invested in it. The government’s health care expenditure, at 1.25% of the GDP, is among the lowest in the world.
The CII-PwC report goes on to list the impact that the NHPM is expected to have on the Indian health care and insurance landscape. “The scheme envisages the adoption of standard treatment guidelines and defined package rates for surgical procedures, and the widespread use of IT and data analytics to monitor scheme implementation and manage fraudulent claims. All these measures taken together will help in regulating the hitherto unregulated hospital and health care sector and in making the health insurance sector a sustainable one. The scheme will help in generating large volumes of data, which may be used later for designing better and targeted health programs. This will assist in effective medical management; in studying the impact of including or excluding specific diseases, populations or coverages; and in optimizing cost and improving efficiencies.”
For Indu Bhushan, CEO of the NHPM, the biggest target is to “significantly reduce the impoverishing impact” of health care expenditures on the poor, along with expanding health care access and improving the quality of care in tier 2 and tier 3 cities and rural areas. “We hope that the program will revolutionize health care in the country,” says Bhushan.
Is It Feasible?
While the intent may be laudable, the big question is whether the NHPM is in fact feasible. Burns sums up the general mood of industry practitioners and analysts: “This is an incredibly ambitious scheme. There are lots of moving parts, and it’s daunting to say the least.”
Take the current health care infrastructure in the country. According to industry estimates, there is less than one doctor and around 1.3 beds per thousand people. Some 70% of health care services are provided by the private sector (which is many times more expensive than the government services), and the majority of the quality health care infrastructure is in the top 20 cities. This basically means that to service the population that the NHPM is targeting, the bulk of which is at present underserved and in rural areas, will require a huge expansion in the delivery system. Also, since the majority of the in-patient beds for tertiary care is from the private sector, it is imperative that the government gets the private sector on board for this scheme.
“Based on data and evidence, if we find that the prices fixed by us are indeed low, we are open to reviewing them.” –Indu Bhushan
“It’s not clear where the money is going to come from. And that, I think, is going to be a critical element that will have to be addressed because, health care being a state subject in India, the central government has heretofore played a minimal role in financing it,” says Burns. Pointing to the Rs. 2,000 crore ($275 million) that has been allocated by the government so far to the NHMP for financial year 2018-2019, Shailender Kumar Hooda, associate professor at the Institute for Studies in Industrial Development (ISID), a New Delhi-based policy research organization, says: “The proposed budget amount will fall short to make the scheme functional, effectively.” Hooda adds that estimates from the National Sample Survey 2014 indicate that the medical bill of the population that is expected to be covered under the NHPM was over Rs. 18,000 crore ($2.4 billion) at current price (i.e., after adjusting for inflation).
Girdhar Gyani, director-general of the Association of Healthcare Providers (India), thinks that the government has not done its homework adequately. He points out that “because of the low premium, many insurance companies have not come forward,” and that the rates of many of the medical procedures listed in the NHPM are “not only low, but completely unviable.” Rana Mehta, partner and leader of the health care practice at PwC, feels that given the low rates, very few service providers would be willing to join in with their existing facilities, let alone build new infrastructure to service the scheme. H. Sudarshan Ballal, nephrologist and chairman of Manipal Health Enterprises, a leading private-sector health care provider, says there is need for “serious dialogue,” and that “reasonable” reimbursement rates need to be worked out.
Bhushan is quick to counter these criticisms, some of which he thinks are “blown out of proportion.” The biggest challenge for him, he says, is the supply-side constraint — how to expand the capacity and improve the quality of services to meet the demand that is going to be created through this scheme. Bhushan concedes that “there is no quick fix,” for this. It will have to be through public-private partnerships, incentivizing the private sector to expand its services and improving the public-sector services. But funding, he insists, is “absolutely not a problem and will largely come from the government’s own resources.” According to Bhushan, the current allocation for the program is notional. It’s a placeholder. He points out that this is the usual practice whenever there is a new scheme. “There is no cap on funding for this project, and we will go back to the ministry for more resources as and when required.” For this year, Bhushan has already asked for an additional Rs. 4,000 crore ($551 million).
“[The government] should push the portability and other such complicated benefits of the NHPM to a later stage and try to make this work at the state level first.” –Atul Gupta
Bhushan’s 35-year career, prior to the NHPM, included being director-general, East Asia Department, at the Asian Development Bank, senior economist with the World Bank Group, and an officer of the Indian Administrative Service. He has a doctorate in health economics and a post-graduate degree in health sciences from Johns Hopkins University. Bhushan is believed to have been handpicked by Modi for the job — which is perhaps why he has the confidence that he will get the resources and the support he needs for seeing it through.
Regarding the pricing of the packages, Bhushan says that the private sector is critical to the success of the scheme, and there is no doubt that the prices offered to them need to be attractive and competitive. At the same, however, it must not lead to a cost escalation in the sector. “We are looking at prices which will not only cover 40% of the population, but will also be a benchmark for the remaining 60%. So we have to be extremely careful. Based on data and evidence, if we find that the prices fixed by us are indeed low, we are open to reviewing them.”
Bhushan now needs to walk his talk. Or else, as Ravi Aron, professor at the Johns Hopkins Carey Business School, cautions, the low rates fixed by the government could result in “adverse selection” of both hospitals that agree to be empaneled in the scheme and doctors that work in these hospitals. “As a result of this twin adverse selection, the quality of care offered to patients under the NHPM may well be much lower than care obtained by patients that pay out-of-pocket,” says Aron.
Dangers of a Top-down Approach
Aron points to another danger: The NHPM is a one-size-fits-all, top-down policy. In a large country with massive disparities, not only will such an approach not work effectively, it will also promote mediocrity. Aron explains: “For innovations and best practices to emerge, it is necessary that many experiments in care delivery should take place. The danger of any centralized and bureaucratic scheme is that it will stifle experimentation and enforce a straight jacketed standardization. There needs to be more thought given to how hospitals will be encouraged to experiment with pricing, patient management, allocation of scarce clinician resources, preemptive and preventive care delivery using IT, etc.”
“The danger of any centralized and bureaucratic scheme is that it will stifle experimentation and enforce a straight jacketed standardization.” –Ravi Aron
There are other challenges, too — for instance, the IT infrastructure that is required to maintain patient records and claims for a national program of this magnitude, especially one that promises portability across states. For the program to be effective, there needs to be a central database which insurers across states can access to verify a person’s eligibility and utilization level. This does not currently exist in India and has to be built from scratch. “This needs to be started in parallel with negotiations with states,” says Gupta. “If different states set up and manage the IT infrastructure individually, this will end up as many different state programs and make portability very challenging, not to mention losing out on scale benefits.”
Gupta observes that experience from earlier health care programs in India suggests that there will be “substantial heterogeneity” across states in “enthusiasm for a central initiative, as well as progress in implementation.” India’s track record in implementing large social/welfare schemes also doesn’t inspire confidence. Recent large initiatives such as demonetization, Adhaar (unique identification) and the goods and services tax have been embroiled in glitches and controversy. ”In my view, they should push the portability and other such complicated benefits of the NHPM to a later stage and try to make this work at the state level first,” says Gupta. Burns suggests that India might be better off piloting this program in a couple of states, one wealthy and one not so wealthy, learn from that and modify the program before rolling it out nationwide.
Unanticipated Consequences
Burns also cautions that there could be some “unanticipated side effects” of pursuing universal health coverage: While the expansion of health insurance will improve access and quality of care, it will also result in skyrocketing health care costs that will necessarily have to be financed. This is because when health insurance coverage is expanded, it encourages the private sector across areas such as technology, pharmaceuticals, med-tech, medical device, hospital supplies, etc., to engage in greater innovation and increase the number of products they develop and sell to the public. While this increases the quality of health care offered, it also increases its cost. This in turn means that the health insurance coverage will need to be continually expanded, not only for the initial target population but also for everybody else, because the cost and quality of health care will keep increasing. “It’s a never-ending cycle,” says Burns. “You have basically created expectations that this coverage is now guaranteed. You will not be able to rescind it. Instead, you will have to reinforce it and buttress it and supplement it going forward. And then it becomes a runaway train.”
“We have to give it some time. It won’t happen overnight.” –Rana Mehta
This has been the experience in the U.S. since the mid-1960s, when it rolled out Medicare and Medicaid for the elderly and the poor. And also in China, which has extended health insurance coverage to over 95% of its population. “[In the U.S.], we’re still dealing with the fallout of how to control health care costs, which rise faster than our country’s economic growth. The problem is also occurring in China. And I fear that India is going to face the same problem. So, you better have a plan for increasing and sustaining economic growth and help finance these health insurance expansions,” says Burns. He adds: “I think people crafting this plan ought to get a second opinion.”
India could also learn from middle-income countries such as Thailand, which is in the process of modernizing its care delivery systems. Says ISID’s Hooda: “Thailand delivers the majority of primary and secondary care in the public health care systems and to a certain extent tertiary care also. For services that are not available in the public system, especially the tertiary care, financial protection has been extended to the entire population. This has resulted in low out-of-pocket expenditure and better outcomes with limited/low public funds. India needs to adopt a similar type of model.”
Crossing the Rubicon
Mehta of PwC offers another perspective. Planning, he says, could go on forever. Sometimes, it’s necessary to take the plunge, tackle the challenges and keep improving. “The imperative for the NHPM is very strong, and I think we have crossed the Rubicon. It’s now about making sure it happens. But we have to give it some time. It won’t happen overnight.”
Aron agrees. The NHPM, he says, is likely to be “bedeviled by crippling shortages in the short term.” Nonetheless, “it is the right way to go. The real benefits of the scheme may come in a time frame of 10 years or more, when health care systems become much more efficient, frugal care delivery mechanisms based on ICT innovations emerge, and the supply of trained clinicians increases.” Hooda believes that the most important aspect of NHPM is its future implications — how will it transform the Indian health care system, and in which direction will it move?
It’s over to Team Modi now.